Community Care Data - Program Integrity Tool (PIT)
Disclosure: This page is a work in progress and information may become out of date quickly. Please check last updated date below each header.
Program Integrity Tool (PIT)
The Non-VA Care Program Integrity Tools (PIT) system is the consolidated source for understanding VA Office of Community Care (OCC) data. PIT collects VA OCC claims data from multiple sources for the purposes of identifying fraud, waste, and abuse. The data is subsequently transmitted for storage in the Corporate Data Warehouse (CDW). PIT provides comprehensive data on all Veteran family member programs, and Choice and MISSION Act utilization.
On February 21, 2023, the Office of Integrity and Compliance (OIC) paused PIT operations, and no claims are available past this date. An archived copy of PIT is available for research data use only.
Archived PIT data is available to research data users on VINCI. Researchers can request data access through the DART research request process. Access to PIT (archived) requires additional steps; instructions are included in the CDW checklist, available on the VHA Data Portal (VA intranet only: https://vaww.vhadataportal.med.va.gov/Data-Access/DART-Request-Process#DocumentsAndForms).
On February 21, 2023, the Office of Integrity and Compliance (OIC) paused PIT operations, and no claims are available past this date. An archived copy of PIT is available for research data use only.
Learn more:
- Office of Integrity and Compliance (OIC) and CREEK’s Guidance for Using Data from the ARCHIVED Program Integrity Tool (PIT) for Researchers
- Memo: Pause of Current Program Integrity Tool (PIT) Operations – PIT will pause ingestion and scoring of VHA Healthcare claims due to data errors identified by staff and VA OIG
PITClaim.ClaimStatus, PITClaim.PayFlag, and PITClaim.CurrentFlag are three fields by which researchers can filter claims to prevent including duplicate or historical claims.
ClaimStatus: Claims with a ClaimStatus of “Approved,” “Paid,” “In Payment,” or “Accepted” should be interpreted as having been approved. Paid claims are also indicated by the PayFlag.
PayFlag = Y will indicate if the claim was paid by VA. If you are interested in looking at acted upon utilization and not only paid claims, you might want to consider leaving out the third filter, PayFlag = “Y”. However, this may leave you with duplicate records.
CurrentFlag = Y will have the most current claim information. If CurrentFlag = N, then the claim is historical.
Please note that we are trying to understand the nuances of many PIT data fields ourselves, but we hope this guidance will help researchers get started.
HSR&D researchers conducted exploratory research using PIT data to analyze health outcomes and costs for cataract surgery. We focused our work on cataract surgery since it is a high-volume procedure, handled exclusively by ophthalmologists, and with well know procedure codes. Below we describe the steps we took to create the research dataset using PIT data.
We extracted FY15 professional and institutional PIT claims data for cataract surgeries using the CPT codes 66982 and 66984. To illustrate how we joined the PIT tables together, we have created two Excel files. One is for the professional component, and the other is for the institutional component.
The PIT data, along with the metadata for these tables, can be found on the VHACDWA01.VHA.MED.VA.GOV server in VINCI. Specifically, these Excel files are adapted from the metadata from [CDWWork].[Meta].[DWViewField]. Our Excel files contain information as of October 2018. For the most up-to-date variables and variable descriptions, please check the original metadata.
Description: Each tab in the Excel files represents a particular PIT table. The yellow rows denote the linking keys between each subsequent table. For the professional component, the orange rows are the variables we chose to keep for our analysis. For the institutional component, this is denoted by the blue rows.
Assumptions: In an earlier analysis, we extracted data using three filters:
- WHERE CurrentFlag = “Y” AND
- ClaimStatus = “Accepted” OR "Approved" OR "Paid" OR "In Payment" AND
- PayFlag = “Y”
This will return current, accepted, and paid claims. If you are interested in looking at acted upon utilization and not only paid claims, you might want to consider leaving out the third filter, PayFlag = “Y”. However, this may leave you with duplicate records.
Caveats: Please note that the PITProcedureCode variable can be messy. In our analysis that focuses on using cataract surgeries, we only found three variations, “66982”, “66984”, and “66.984” when we intended to search for CPTs 66982 and 66984. We assume that “66.984” is a data entry error for “66984”. Thus, it was relatively easy to re-code “66.984” to lump with the “66984” records. However, users should be aware that the data could be more complex when one expands to other procedure codes that might contain typos and/or other variations.
Additionally, we found that only ~ 40-50% of institutional and professional claims from FY15-18 have non-missing SSN and PatientICN in the [CDWWork].[SVeteran].[PITPatient] table. This figure is for all claims and not only cataracts. However, we discovered that the MemberID variable in SVeteran.PITPatient actually contains the patient’s SSN as well. This variable is rarely missing. Thus, MemberID is recommended to be used as a patient identifier.
We are unaware of an official variable that defines an inpatient record in PIT. For our analysis, we used PITBillTypeCode, PITPlaceOfService, and RevenueCode to classify records. PITBillTypeCode and PITPlaceOfService indicate the type of location where a service/diagnosis was received. RevenueCode indicates the type of charges on a claim, and sometimes these charges can be for inpatient beds. For code definitions, please see public documentation including that from ResDAC and CMS. Most inpatient stays can be captured with revenue codes < 230, place of service (POS) codes 21, 51, 56, and 61, and Billtype code 11x and 12x. Some researchers may want to include additional codes based on their research question. We recommend reviewing all codes when creating your analysis plan.
Additional information is available from the Community Care Research Evaluation & Knowledge (CREEK) Center. CREEK provides detailed documentation on one approach for finding hospital inpatient stays in PIT.
The Community Care Research Evaluation & Knowledge (CREEK) Center provides guidance, including sample SQL queries, for finding outpatient visits in PIT.
PIT data contain the National Provider Identifier (NPI), which can be found in the Claim_Provider table. NPI is a unique 10-digit identification number issued by the Centers for Medicare and Medicaid Services to all health care providers in the United States.
Researchers can link NPI to providers in VA and Medicare using the National Plan and Provider Enumeration System (NPPES) Downloadable File from The Centers for Medicare and Medicaid Services (CMS). https://www.cms.gov/Regulations-and-Guidance/Administrative-Simplification/NationalProvIdentStand/DataDissemination.html. NPPES data are also available for research projects in CDW on the SAS Grid using libname CMS_PBLC. Note that these data are only available on the Research Grid.
NPPES data can change week to week to reflect changes in provider information; for example, the data is updated when a provider moves. In general, however, the data are static. From these data, researchers can learn information about the provider such location, gender, and provider type and can perform specialized analyses such as geocoding.
NPI is also available within the VA CDW SStaff table, although we caution researchers against using NPI in SStaff.SFeeVendor. HERC researchers have encountered errors with NPIs being attributed to the incorrect physician.
Records are broken down to different levels in VA data and PIT data. On the VA side, each record represents an encounter (i.e. everything that occurred during an interaction between a patient and medical professional). On the PIT side, each record represents a claim, and there can be multiple claims during one encounter (for example, labs and procedures that occurred during the same encounter could have different claims). Researchers will need to roll-up the claims to the encounter level to make costs comparable.
In order to roll up claims to the encounter level, researcher will first need to identify all records within the claim. We recommend using PITClaimSID to identify all records for one claim. Researchers may also want to sort on PITClaim.CurrentFlag, PITClaim.ClaimStatus, and PITClaim.PayFlag to make sure no erroneous or historical records are included. Next, use a combination of PITPatientSID, admission and discharge dates to identify records within an encounter.
There are two types of code sets that can be referred to as Procedure codes. Service codes (CPT and HCPCS codes) are at line level; ICD Procedure codes are at claim level.
Below is the SQL code to identify both Procedure code sets.
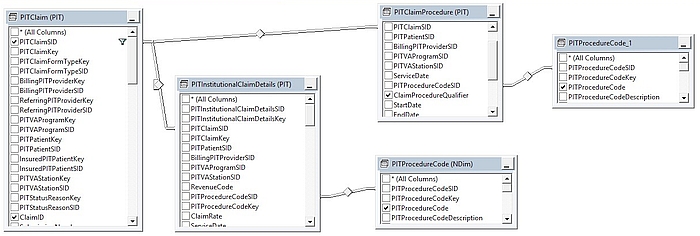
SELECT TOP (200) PIT.PITClaim.PITClaimSID, NDim.PITProcedureCode.PITProcedureCode AS ServiceCodes, PIT.PITInstitutionalClaimDetails.ClaimPosition, PIT.PITClaimProcedure.ClaimProcedureQualifier, PIT.PITClaimProcedure.ProcedureDate, PITProcedureCode_1.PITProcedureCode AS ICDProcCOdes, PIT.PITClaim.ClaimID, PIT.PITClaim.PatientAccountNumber, PIT.PITClaim.ClaimStatus, PIT.PITClaim.CurrentFlag, PIT.PITClaim.PITClaimBatchLogKey
FROM NDim.PITProcedureCode INNER JOIN
PIT.PITInstitutionalClaimDetails ON NDim.PITProcedureCode.PITProcedureCodeSID = PIT.PITInstitutionalClaimDetails.PITProcedureCodeSID RIGHT OUTER JOIN
NDim.PITProcedureCode AS PITProcedureCode_1 INNER JOIN
PIT.PITClaimProcedure ON PITProcedureCode_1.PITProcedureCodeSID = PIT.PITClaimProcedure.PITProcedureCodeSID INNER JOIN
PIT.PITClaim ON PIT.PITClaimProcedure.PITClaimSID = PIT.PITClaim.PITClaimSID ON PIT.PITInstitutionalClaimDetails.PITClaimSID = PIT.PITClaim.PITClaimSID
WHERE (PIT.PITClaim.PITClaimSID IN (290419263, 221255198))
Figure 1. Identifying Procedure Codes in PIT
Under the MISSION Act, eligible Veterans can receive urgent care from in-network urgent care providers.
Initially, the Urgent Care Benefit was provided to Veterans through the Patient-Centered Community Care (PC3) Contract, and the Third-Party Administrator was TriWest. Beginning March 2020, the urgent care benefit will begin transitioning to VA Community Care Network (CCN) contracts. On March 18, 2020 Region 1* will be the first region to transition; Optum will administer the benefit. Eventually, the Urgent Care benefit will transition to CCNs for Regions 2-6 as well. Optum will administer the contracts for Regions 2 and 3. Region 4 will be administered by TriWest. Regions 5 and 6 are still pending.
Urgent care claims are those billed with CMS Place of Service (POS) codes 17 or 20. The urgent care claims data is received from two sources: VA Financial Service Center (FSC) and 10D/Office of Community Care’s (OCC’s) Informatics/Data Analytics' (IDA) team. IDA extracts the urgent care claims data from PIT. IDA is in the process of developing a PowerBi dashboard on Urgent Care data that hopefully can be used by researchers in the future.
Visit the VHA Office of Community Care (OCC) website to learn more about the urgent care benefit https://www.va.gov/COMMUNITYCARE/programs/veterans/Urgent_Care.asp. Resources on care under the MISSION Act and the transition to CCNs are available on the VA OCC intranet site: https://vaww.va.gov/COMMUNITYCARE/cchub/missionact.asp.
*A map of states included in the CCN regions is available on the OCC website.
Background: We wish to estimate the total cost for a CHOICE cataract surgery that was performed in FY18. Our initial analyses showed that the mean cost was much lower than we expected, especially compared to a cataract surgery performed at a VA hospital. Thus, we developed three algorithms to clean and process the data. Ultimately, we will compare mean/median costs across the three algorithms.
INCLUSION criteria for all algorithms:
- FY18 claims found in the CDW PIT data
- Claim must be current, paid, and accepted
- CPT code for the cataract is either 66982 or 66984
EXCLUSION criteria for all algorithms:
- Claims that contain a CPT modifier value of 55 (post-operative care)
- Claims that contain a CPT modifier value of 56 (pre-operative care)
- Claims that contain a CPT modifier value of 79 (unrelated procedure or service performed by the same physician during the post-operative period)
NOTES:
It is important to extract the PITPlaceOfService variable. This variable can be obtained by linking PITPlaceOfServiceSID to [CDWWork].[NDim].[PITPlaceOfService]. Our analysis concentrates on records with Ambulatory Surgical Center (ASC), Outpatient Hospital, and Office places of service.
Algorithm A:
Dataset is at the patient x surgery date x CPT x eye side x PITPlaceOfService level
Surgeries that have no eye side information are excluded
A concordance variable (CONCORDANCE) is created:
- CONCORDANCE = 1 if the number of records is equal to the expected number of records for the type of claim, based on PITPlaceOfService
- CONCORDANCE = 2 if the number of records is more than the expected number of records for the type of claim, based on PITPlaceOfService
- CONCORDANCE = 3 if the number of records is less than the expected number of records for the type of claim, based on PITPlaceOfService
- CONCORDANCE = 4 if the type of claim is not expected, based on PITPlaceOfService. For example, this could be an institutional record for a cataract surgery with an ASC place of service. Typically, over 99% of ASC records are professional claims.
- Records with CONCORDANCE = 1 are prioritized
Costs were calculated according to these rules:
- PITPlaceOfService = Office - take the highest professional cost
- PITPlaceOfService = ASC - take the highest professional cost
- PITPlaceOfService = Outpatient Hospital - take the highest institutional and the highest professional cost and sum together
Algorithm B:
Dataset is at the patient x surgery date x CPT x eye side x PITPlaceOfService level
All records are kept irrespective of eye side modifiers
If eye side is missing, sum all costs for that day
A concordance variable (CONCORDANCE) is created:
- CONCORDANCE = 1 if the number of records is equal to the expected number of records for the type of claim, based on PITPlaceOfService
- CONCORDANCE = 2 if the number of records is more than the expected number of records for the type of claim, based on PITPlaceOfService
- CONCORDANCE = 3 if the number of records is less than the expected number of records for the type of claim, based on PITPlaceOfService
- CONCORDANCE = 4 if the type of claim is not expected, based on PITPlaceOfService. For example, this could be an institutional record for a cataract surgery with an ASC place of service. Typically, over 99% of ASC records are professional claims.
- Records with CONCORDANCE = 1 are prioritized
Costs were calculated according to these rules:
- PITPlaceOfService = Office - take the highest professional cost
- PITPlaceOfService = ASC - take the highest professional cost
- PITPlaceOfService = Outpatient Hospital - take the highest institutional and the highest professional cost and sum together
Algorithm C:
Same as Algorithm B above, except records where cost is less than $200 are dropped from the analysis
Note: We know that some of the costs appear to be too low, therefore we chose $200 as a ballpark figure that is approximately a little higher than the cost for the average pre-operative visit.
Conclusions: The analyses reflect that there were 23,000 – 24,000 cataract surgeries paid by Choice in FY18. It is encouraging to see that the mean and median costs (as well as the interquartile range) are quite similar between the three algorithms. Typically, the mean cost for a cataract surgery ranged from $600 - $900 for surgeries performed at an ASC or in an office. For surgeries performed at an outpatient hospital, the mean cost is ~ $1,800. Median costs were only barely higher than the mean costs across all algorithms and places of service.
The payments we found were just for the cataract surgery. This does not include other procedures that may have been done with the cataract, such as anesthesia. The PIT claims detail is like an à la carte menu. Each service has a bundle of possible procedures, so it is critical to understand the bundle—in this case, we just found the cost of the cataract CPT. We used the PIT authorization ID to find other CPT codes that share the same authorization. Unfortunately, the PIT authorization ID is sometimes used for services that may not be related to the cataract. For example, a patient had acupuncture and cataract with the same authorization ID. We used VA data to see what CPT codes were used simultaneously with a cataract CPT; this allowed us to create a possible list of ancillary CPT codes. We then used the PIT authorization ID merged with the list of possible ancillary CPT codes to find likely ancillary costs. This worked reasonably well, but it was time consuming.
The PIT Data Repository was developed by IBM and is comprised of three major components: WebSphere Operation Decisions Management, Fraud Abuse and Management System, and the Claims Scoring Tool that applies business logic to inbound claims. The PIT aggregates many sources of data and allows for checking for fraud, waste, and abuse pre-payment where a bi-directional feed exists. PIT also receives terminal state paid data to perform post payment analytics. Beginning FY2016, Choice data began processing outside the Fee Basis Claims System (FBCS) in the Plexis Claim Management system (PCM). The Department of Program Integrity with OI&T and Contract team maintain this system and its functions.
PIT is considered a transaction database; the data flow into PIT begins with the various claims adjudication and processing systems transmitted claim data to the PIT data repository. These systems include but not limited to FBCS, PCM, eCAMS, CCRS, and CP&E. Non-VA providers and Third Party Administrators (TPAs) submit EDI837 files to EMDEON and from there it goes into ERepos in VA, then to FPPS to FBCS and finally to PIT. The Department of Program Integrity has created standardized fields for PIT to perform FWA detection activities. Data that flows to PIT from sources systems may vary somewhat based on new data attributes and requirements for additional data elements established during the development of the source system feed.
The PIT Domain was released into the CDWWork environment on September 25, 2018. The domain has 67 views, 27 dimensions, and 40 fact views. The PIT domain contains VA claims that have been processed through the PIT, including but not limited to Choice claims. CDW documentation includes:
- PIT Release documents (VA intranet only: https://vaww.cdw.va.gov/metadata/Metadata%20Documents/Forms/AllItems.aspx?RootFolder=/metadata/Metadata%20Documents/PIT%201.0&FolderCTID= 0x0120007BD83FE7EC890F42B79E1DA11A744B1E&View=%7bA9968955-5886-4DEC-A6BF-0CB219ADD175%7d)
- CDW Metadata Report (VA intranet only: https://vaww.cdw.va.gov/metadata/_layouts/15/ReportServer/RSViewerPage.aspx?rv%3aRelativeReportUrl=/metadata/Reports/Metadata%20Report.rdl&Source=http%3a//vaww.cdw.r02.med.va.gov/metadata/ Reports/Forms/AllItems.aspx&DefaultItemOpen=1)
- How to Get Access (VA intranet only: https://vaww.cdw.va.gov/Pages/CDWHome.aspx; select "Data Access Information")
We have summarized 11 different methods for identifying Choice claims in the PIT tables. Below is a file that shows you the T-SQL search strings for each method. Please note that the summary table figures were calculated on 2/13/2019. Since PIT data are active and updated nightly, the numbers may have changed slightly.
Prior to FY20, we recommend that PIT data be analyzed in combination with Purchased Care/Fee data for a complete understanding of VA Community Care utilization and costs. Starting January 1, 2020, all Community Care data will be found in PIT or the CDW Purchased Care Domain (CDW FEE schema).
VA payments to non-VA providers are limited to Medicare payments, by law. In general, providers can bill VA whatever amount they feel like and it is up to the TPA, VA, or FSC to ensure the billed amount is correct, prior to releasing payments. Choice and PC3 payments should be based on the Medicare rates times the CLIN (which can be 85%, 100%, 150%, 250%, and a few other multipliers, based on the provider contracts) but the price validation was not set up during the initial processing of Choice and PC3 claims, so VA paid the billed amounts on submitted claims. The result is that for a single CPT code, you may find different payments which vary from a couple hundred dollars to tens of thousands of dollars. Since the onset of Choice there have been efforts to go back to reprice and collect money from overpayment to providers but it is a time-consuming effort and is being remedied moving forward.














